Powerful new tools have transformed prosthetic 3D design in recent years. Software like Solidworks, Fusion360, MeshMixer, and ReCap Photo harmonize affordability, customization, and iterative design, reshaping prosthetics for the better. Integrating 3D scans introduces even more precision, allowing for tailor-made prosthetics that align seamlessly with each patient’s needs.
Here we explore the challenges, methodologies, and best practices of the design process, and show how interdisciplinary collaboration plays a crucial role in the creation of innovative prosthetics.
The role of software in prosthetic 3D design
The modern landscape of prosthetic design has been revolutionized by a suite of powerful software applications, ushering in an era of innovation and cost-effective solutions. Solidworks, Fusion360, MeshMixer, and ReCap Photo stand at the forefront of this transformation, each playing a distinctive role in shaping the journey from concept to creation.
Solidworks, a prominent CAD software, empowers designers with an extensive array of tools to craft intricate 3D models of prosthetic devices. With its versatile features, Solidworks facilitates not only visualization but also simulations and the integration of advanced components. The program propels the development of sophisticated prosthetics, as Philip Jonah Ezigbo at the Federal University of Technology Owerri and team wrote in a paper published in 2019 in the International Journal of Mechatronics, Electrical and Computer Technology.
Further Reading: Are 3D-Printed Prostheses the Solution for Limb Loss in Low-Income Countries?
Another research team, Aarav Patel at Rutgers University and colleagues, aimed to engineer a functional and affordable 3D-printed prosthetic hand that is accessible to the general population. The design was constructed and simulated in SOLIDWORKS (CAD) software, and further studies were conducted to determine a material and part composition that would yield functionality, durability, and affordability. They published their results in 2020 at the IEEE MIT Undergraduate Research Technology Conference.
Fusion360, another robust CAD tool, takes collaboration to new heights by supporting interdisciplinary teamwork while offering parametric modeling and simulation capabilities. Its synergy with 3D printing expedites the transition from virtual designs to tangible prototypes, as in the image below. A. Iwuoha and colleagues published these findings in 2020 in the International Journal of Engineering and Innovative Technology (pdf).

This 3-D printed prosthetic hand was printed and assembled by FDA researchers in their CDRH laboratory. Similar devices are also available on the internet and are typically used for children born without fingers. Photo: US Food and Drug Administration (free of copyright)
The researchers employed 3D printing technology to produce a body-powered prosthetic limb for a 12-year-old amputee. The design was made to be parametrically scalable to appropriately size the wearer. Fusion 360 software was used for the design, and the prosthetic limb was 3D printed using a flexible filament thermoplastic polyurethane. The prosthetic limb is body-powered and activated by moving the residual limb to achieve a grip (see the image below).
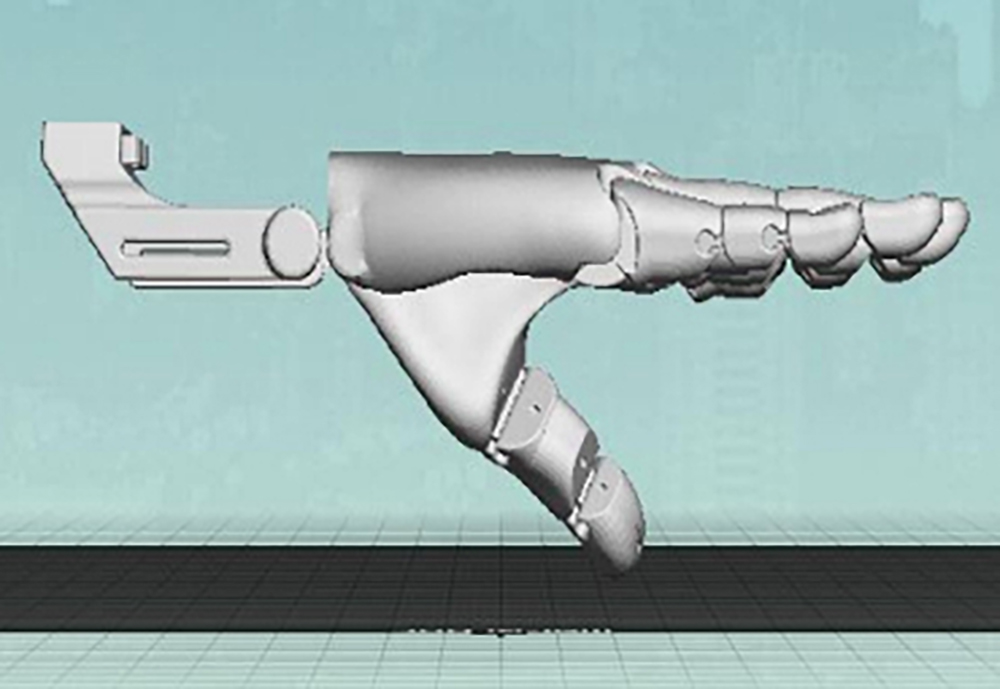
Side view of the Prosthetic Hand 3D model in Fusion 360. Image: Iwuoha & Iheme, 2020
MeshMixer, tailored for 3D mesh manipulation, refines prosthetic geometries. Sculpting, smoothing, and mesh optimization ensure prosthetics are lightweight, comfortable, and aesthetically pleasing, according to Daniel Panchik at Elizabethtown College and team, who published the results of a case study in 2021 in the Internet Journal of Allied Health Sciences and Practice.
The case study explores the ease of using task-specific design in computer-aided, open-source 3D printed design software. The study involved recruiting participants and assessing their needs to guide the prosthetic designs. Hand measurements were obtained and entered into computer software to create computer-aided design drawings of the digit prosthetics. The collaboration between occupational therapy and engineering disciplines resulted in customized 3D-printed finger prosthetic designs to meet the participants’ specified tasks.
Taking a look at ReCap Photo, it introduces a new dimension through photogrammetry, creating precise 3D models from photographs. Particularly valuable for capturing residual limb shape and dimensions, ReCap Photo contributes to accurate customization, bypassing conventional casting methods.
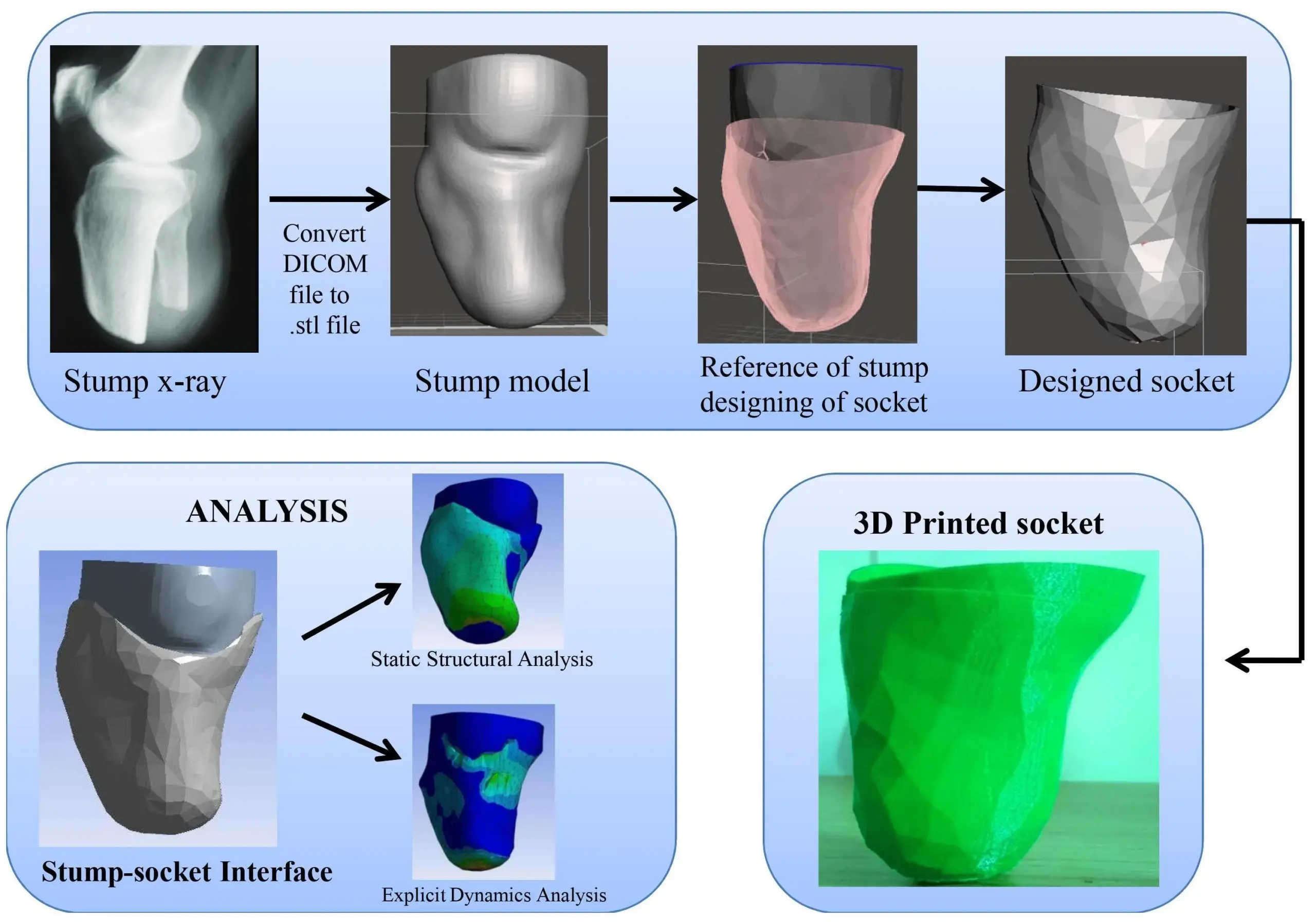
CT-based 3D models obtained from image processing software and modified in CAD modeling software in STL format.
Image: Gubbala & Inala, 2021 (CC by 4.0)
Rilo Berdin Taqriban at the University of Diponegoro and colleagues presented the development of a transtibial prosthetic socket using photogrammetry using ReCap Photo Utilities and Meshmixer in a paper published in 2019 at the International Seminar on Research of Information Technology and Intelligent Systems. The 3D model of the socket is created by taking photos of the remaining limb of the amputee and processing them in software for 3D generation and rectification. 3D printing is used to print the socket, which is then compared to a conventional casting socket using image processing.
Similarly, Giri Ratnakar Gubbala and Ramu Inala used CT-based 3D models and examined them in ANSYS simulation to perform static and dynamic analysis of the prosthetic stump and socket (see the image above). They proposed the use of 3D printing technology and finite element-based simulation and analysis for the overall prefabrication evaluation system to allow healthcare providers to provide comfortable prosthetic sockets for lower limb amputees.
Together, these software applications redefine the prosthetic landscape by enhancing affordability, customization, and iterative design. The fusion of software prowess and 3D printing significantly curtails costs while enabling personalized designs that align with individual patient needs. This transformation underscores the shift from traditional methods to efficient, patient-centered prosthetic solutions.
The challenge of working with 3D scans
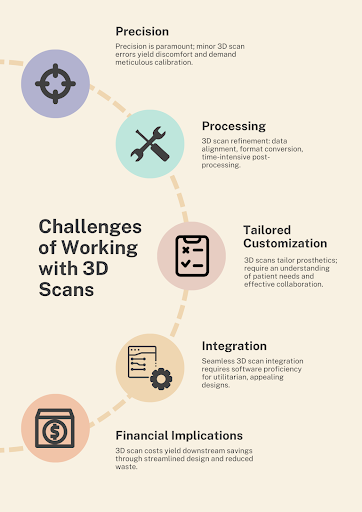
The incorporation of 3D scans into the prosthetic design process presents a revolutionary avenue laden with advantages, yet demands astute navigation through intricate challenges. The utilization of 3D scans calls for meticulous attention to a series of pivotal factors.
Precision: The pivotal role of precision in prosthetic design cannot be overemphasized. Even minor discrepancies in 3D scans can lead to discomfort or operational deficiencies. Achieving accuracy hinges on the meticulous calibration of scanning tools and optimal patient positioning during the scanning process, according to Taqriban and colleagues.
Processing: The journey from raw 3D scans to usable models involves intricate post-processing. Tasks encompass data refinement, alignment of multiple scans, and data format conversion for CAD software or 3D printing, accorind to Panchik and colleagues. This phase necessitates time and specialized knowledge, underlining the intricate nature of the process.
Tailored Customization: 3D scans are a gateway to tailored solutions that harmonize with individual patient needs. However, crafting personalized prosthetics demands a comprehensive understanding of patients’ functional requisites, lifestyles, and preferences. Effective collaboration with both patients and healthcare experts is essential to ensure the symbiosis of form and function, Panchik and colleagues write.
For example, Panchik’s paper underscores the paramount significance of tailored customization in prosthetic design. Task-specific design effortlessly integrates into computer-aided, open-source 3D printed design software, enabled by a fruitful collaboration between occupational therapy (OT) and engineering disciplines. Hand measurements fuel computer-aided design drawings, crafting personalized 3D-printed finger prosthetic designs. The study accentuates customization through interdisciplinary teamwork, leveraging both subjective and objective measures to create solutions that seamlessly align with participants’ specific tasks. The ease of incorporating technology further amplifies the paper’s spotlight on crafting prosthetics tailored to individual needs.
Integration: Seamlessly weaving 3D scans into the design realm mandates adeptness with software applications such as Solidworks and Fusion360, Ezigbo and colleagues write. The intricacies of software proficiency must be mastered to generate prosthetic designs that are both utilitarian and visually pleasing.
For instance, Eziigbo’s paper explains how to seamlessly integrate 3D scans into the design process via these steps: Photogrammetry captures limb images from various angles, and software stitches them into a 3D model, accurately representing the limb. The 3D printed socket is compared to a conventional cast version, evaluating fit and function through image analysis. Real-world testing assesses comfort and functionality during walking, spotlighting the synergy of 3D scans and CAD design in prosthetic innovation.
Financial Implications: The initial expense of 3D scanning equipment and software can be daunting, yet these investments bear the potential for downstream cost savings. By refining the design process, diminishing material wastage, and negating costly manual adjustments and conventional casting methods, 3D scans ultimately engender economic advantages, Ezigbo writes.
In summary, 3D scans within the prosthetic design framework offer a corridor to customization, accuracy, and affordability. Yet, this pathway necessitates a judicious examination of the articulated challenges to forge prosthetic devices that harmonize seamlessly with patient needs, culminating in functional, comfort-infused, and aesthetically pleasing solutions.
Maximizing efficiency with residual limb measurements
Efficiency in the prosthetic design process, solely reliant on residual limb measurements, hinges on strategic methodologies and best practices. The following considerations epitomize this pursuit.
Precision in Measurement: Attaining precision mandates reliable measurement techniques. Be it calipers, tape measures, or advanced devices like 3D scanners and bioimpedance analyzers, accuracy is paramount to acquiring dependable residual limb measurements.
Lucy Armitage at the University of New South Wales and colleagues highlight measurement precision in a paper published in 2019 in the journal Prosthetics and Orthotics International. The research evaluates iSense scanner reliability and validity for transtibial residual limb volume. Assessors measured 13 models, showing excellent intra-rater and most inter-rater reliability, emphasizing precision. Criterion validity was poor, revealing accuracy challenges. The study underscores the significance of precise measurement in prosthetic design. Reliable tools like the iSense scanner ensure accurate residual limb volume measurements. The paper’s framework aids in assessing measurement tools’ reliability and validity, bolstering measurement precision in prosthetic design.
Uniform Protocol: Homogenizing measurement protocols heightens consistency, permitting cross-patient and cross-session comparability. Standardizing anatomical landmarks, measurement points, and positioning ensures coherent data collection, according to Robert Youngblood at Washington University and colleagues in their paper published in 2020, also in Prosthetics and Orthotics International.
The research focuses on the uniform protocol challenge. It employs a fixed-order crossover design with standardized out-of-laboratory activity, ensuring consistent measurement of residual limb fluid volume. Transtibial amputees used elevated vacuum and suction suspension in two sessions, with in-socket fluid volume continuously measured. The paper underscores uniformity’s significance in prosthetic research, aiding precise measurement across patients and sessions. The standardized protocol offers insights into elevated vacuum’s effectiveness in volume management during activity. This emphasizes the importance of standardized protocols in advancing prosthetic design and fitting.
Meticulous Documentation: Detailed records of measurements, encompassing technique specifics, measurement points, and patient information, provide a compass for future referencing. This record-keeping is instrumental in tracking changes, subsequently streamlining design and fitting endeavors.
Synergy with Software Tools: The integration of software tools optimizes the process. CAD software like Solidworks and Fusion360 facilitate 3D model creation from measurements, enabling virtual design and customization. Tailored software such as MeshMixer and ReCap Photo further fine-tune models, yielding accurate residual limb representations.
Wireless soft sensors can monitor pressure and temperature between the residual limb and prosthesis, as described byJean Won Kwak at Northwestern University and colleagues writing in the journal Science Translational Medicine in 2020. Sensors wirelessly communicate with devices during activities. This integration enables constant monitoring, aiding fitting and detecting dangerous pressure and temperature changes. The paper contrasts rigid conventional sensors with wireless soft ones, addressing comfort issues. By combining wireless technology and soft sensors, the study underscores the potential for enhanced comfort and accuracy in prosthetic design and fitting.
Iterative Development: Measurement-guided iterative design enables custom-tailored prosthetics. By embedding measurements in the design, devices are crafted to mirror residual limb dimensions. Rigorous prototype testing based on these measurements ensures optimal fit and function, Youngblood and colleagues write.
Collaboration and Communication: Effective interplay between prosthetists, designers, and patients is pivotal. Prosthetists offer functional insights, patients’ input ensures comfort, and designers translate measurements into functional solutions.
Implementing these methodologies and best practices culminates in an efficient prosthetic design process anchored in residual limb measurements. The fusion of precision, uniformity, documentation, software integration, iterative design, and collaborative engagement converges toward personalized, functional, and successful prosthetic solutions.
The collaborative approach to prosthetic 3D design
A harmonious alliance between prostheticians, clinicians, and biomedical engineers serves as the bedrock for groundbreaking advancements in prosthetic design and development. The potency of interdisciplinary collaboration manifests through the following avenues.
Spectrum of Expertise Integration: The convergence of engineering, materials science, biomechanics, and healthcare is pivotal. The synergy of these fields, coupled with cutting-edge technologies like 3D printing, artificial intelligence, and virtual reality, engenders innovative solutions attuned to the heterogeneous needs of users, according to a paper by Kai Xu and Shengfeng Qin published in 2023 in Actuators.
Task-Centric Design: The fusion of occupational therapy (OT) with engineering begets bespoke 3D-printed finger prosthetics, attuned to specific tasks. The fruitful marriage of these realms finds expression in open-source 3D design software, streamlining the creation of task-specific prosthetic solutions, Panchik writes.
Educational Empowerment: Infusing prosthetic design and manufacturing into educational curricula within engineering and life sciences opens vistas. Such educational exposure not only simplifies access to functional prosthetics but also augments their widespread adoption among users, according to Faruk Ortes and colleagues, writing in a paper in 2016 in The Eurasia Proceedings of Educational and Social Sciences.
Affordability Amplified: The collaboration between biomedical engineers and clinicians yields functional and economically viable 3D-printed prosthetics. These designs, birthed in computer-aided design (CAD) software, combine optimal material composition with cost-effectiveness without compromising utility, Patel writes.
Smartphone-Enabled Telemedicine: A marriage of biomedical engineering and clinical acumen culminates in ingenious methods for affordable prosthetic fabrication. Leaning on the ubiquity of smartphones, this approach democratizes access to prosthetic care, especially in underserved regions, according to Isaac Cabrera at the University of San Diego and colleagues who published a paper in 2020 in TechRxiv.
Collectively, interdisciplinary collaboration emerges as the linchpin in the prosthetic design landscape. The marriage of expertise, task-centric solutions, education, affordability, and smartphone-driven innovations underscores its transformative potential. Through this multifaceted prism, the partnership between prostheticians, clinicians, and biomedical engineers unveils a realm of innovative solutions tailored to the myriad demands of diverse users.
Further reading
About the author
Esther Ivanova Matamoros Alcivar is a former Engineering for Change Fellow and a biomedical engineer based in Ecuador.

